Children's ward
Children's ward
Children's ward is a special ward within Specialized Rehabilitation Hospital Banja Koviljaca. It was founded on March 1st 1989 and it is the first of its kind in Serbia. It is located in a separate building with around 100 beds for the accommodation of children and their parents. Within the same building, all therapeutic procedures are performed, including two kinesiotherapy rooms - for babies up to 2 years and the other for older kids. There are also occupational therapy, electrotherapy, hydro-kinesis performed in swimming pools or Hubbard tank, underwater massage, parafin application. In our Sulphur Bath, for children older than 12 months, sulphuric peloid of Banja Koviljaca is applied. Peloid is unique in the world by its composition and it gives excellent results in treating various diseases of locomotor pparatusin children.

Indications for children rehabilitation

Indications for children rehabilitation
We are equipped with US diagnostics and EMNG equipment which are operated by our physicians being supported by professors from the clinics in Belgrade. Cooperation and experts’ supervision is realized with the University Children’s Hospital, Institute for Mother and Child, Institute for Orthopedic Surgery Banjica, Institute for Rheumatology and Child and Adolescent Neurology and Psychiatry Clinic in Belgrade.
We are equipped with US diagnostics and EMNG equipment which are operated by our physicians being supported by professors from the clinics in Belgrade. Cooperation and experts’ supervision is realized with the University Children’s Hospital, Institute for Mother and Child, Institute for Orthopedic Surgery Banjica, Institute for Rheumatology and Child and Adolescent Neurology and Psychiatry Clinic in Belgrade.
We are equipped with US diagnostics and EMNG equipment which are operated by our physicians being supported by professors from the clinics in Belgrade. Cooperation and experts’ supervision is realized with the University Children’s Hospital, Institute for Mother and Child, Institute for Orthopedic Surgery Banjica, Institute for Rheumatology and Child and Adolescent Neurology and Psychiatry Clinic in Belgrade.
We are equipped with US diagnostics and EMNG equipment which are operated by our physicians being supported by professors from the clinics in Belgrade. Cooperation and experts’ supervision is realized with the University Children’s Hospital, Institute for Mother and Child, Institute for Orthopedic Surgery Banjica, Institute for Rheumatology and Child and Adolescent Neurology and Psychiatry Clinic in Belgrade.
Balneotherapies beneficial for children

Peloid has excellent results in treating some children diseases, and it is much less aggressive than medicines and surgery. In modern medicine, there is a tendency to avoid aggressive methods, starting with medicines and surgery to various radiations, particularly if these cause allergies and other complications. On the other hand, balneotherapy uses natural non-invasive factors which provides children a chance for more quality treatment without accompanying consequences.
For several decades, sulphuric peloid of Banja Koviljaca has been successfully applied in management of different locomotor diseases in children. Its great therapeutical abilities have been scientifically proved, and positive effects have been demonstrated in scientific papers prepared by Banja Koviljaca’s experts done with our little patients who come to the specialized Children’s Department every day.
Peloid has excellent results in management of some diseases in children, such as bone fractures at all levels, aseptic bone necrosis, femoral head epiphysiolysis, joint contractures, milder impairments of peripheral nerves, recovery after surgeries on locomotor system, rheumatic diseases in their remission phase. Good results have been achieved in treatment of children with cerebral paralysis, if damage is minor and if peloid therapy is applied from 2 years of age regularly with repeating series of therapies.
How do therapies for children look like?
Peloid is applied locally directly onto the skin (as wet heat) on some segments. Peloid temperature is 38-40°C. It is applied for 20 minutes, followed by rinsing, rest, and kinesitherapy, respectively. Maximum number of application per a series is 20, this is followed by two-week break, and then the series is repeated.
In resistant contractures, regardless its etiology, kinesitherapy in peloid is applied (shoulder, elbow, knee, ankle). Peloid is first applied onto the impaired joint, followed by 10-minute exercises aimed to increase range of motion.
The unique treatment for children in the world

Application of sulphuric peloid of Banja Koviljaca in children is unique in world’s balneology.
Application of sulphuric peloid in children has been based on empirical and scientific knowledge for over a century. Since the Children’s Department was open in Banja Koviljaca, application of sulphuric peloid has been done as per severe indications with expert supervision of University Children’s Hospital, Institute for Mother and Child, Institute for Orthopedic Surgery Banjica from Belgrade.
Our experience gained through many years demonstrate that we have excellent results in treating children with injuries and anomalies of locomotor system, which is evidenced by many scientific papers presented in our country as well as worldwide. By continuously following events in the balneology world, we are proud that due to unique properties of Banja Koviljača’s peloid, nowhere in the world this kind of efficient treatment may be provided.
When is peloid applied in children?

Perthes disease

Legg-Calve-Perthes disease most often occurs between 4 and 10 years of age, although the disease may develop earlier and later. It more frequently occurs in boys than in girls. A cause of disease is sill unknown, but it is known that the disease develops as a consequence of repeated vascular interruptions, i.e. infarctions in femoral head. The dead bone is reabsorbed, and at its location a new one is created. This process lasts from 3 to 5 years.
Clinically, the disease is manifested with a pain in the hip region, usually expanded towards knee, and sometimes it happens that the first symptom of the disease is pain in the knee, not in the hip. Moreover, limping, hip and upper leg muscles hypotrophy, limited hip motion are present. The most common consequence and complication is early hip coxarthrosis.
Outcome and prognosis of the disease mostly depend on the age when the disease occurred, on the level of initial damage, on gender, as well as on time between the onset of the disease and commencement of treatment. In younger children and boys, prognosis for the disease is better.
Treatment may be non-surgical and surgical, and a decision on the treatment mode is made based on aforementioned factors. Physical therapies are applied both in non-surgically and surgically treated children. Physical treatment is used to improve blood circulation in the hip region and hence contribute to acceleration of femoral head recovery, to contribute strengthening of muscles and establishing full motion range and to relieve pain in hip and knee regions. For this, electrotherapy for pain relief are applied, then kinesi and hydrokinesitherapy (exercises and exercises in water) and therapy with sulphuric peloid.
Juvenile idiopathic arthritis - JIA

Children rheumatism was mentioned in records in XVI century in England, and the first demonstrations of children with acute and chronic arthritis were provided in XIX century. Dr Still was the first to publish clinical characteristics of children with arthritis. One of the most severe forms of this disease is even called after him – Still’s disease. As per the latest classification from 1997, JIA has to start prior 16th birthday, localized in one or several joints continuously for 6 weeks with excluding other rheumatic and non-rheumatic diseases.
This is a severe disease leading to invalidity. A cause of JIA is not completely clarified. Some bacterial and viral infections, then genetics, stress – psychical trauma, changed immune response are all mentioned. Clinical picture include swelling of one or several joints.
Treatment includes medicines and physical therapies. From the very onset of the disease, in addition to medicines, physical therapies and rehabilitation should be initiated as well. For each child, an individual rehabilitation plan and program is prepared depending on a stage, disease activity level and severity of changes in joints.
AIM OF THERAPIES:
- Positioning of joint into optimum functional position
- Pain relief and reduction of inflammation of the affected joint
- Prevention of deformities and contractures
- Prevention of muscle hypotrophy, increase of muscle strength
- Preservation of respiratory muscle function
- Maintaining abilities for everyday life
In the management of this severe disease, there is a team consisting of a children’s rheumatologist, children’s physiatrist, physical and occupational therapist, nurses, children’s orthopedist and parents.
Children suffering from JIA referred by a children rheumatologist, Institute for Mother and Child, and University Children's Hospital come to our Hospital. There are children of different ages, with made diagnosis and initiated treatment with medicines. Many of these children, in addition to arthritis, already have contractures, expressed muscle hypotrophy, impaired body posture. Because of pain, a child finds a position with least felt difficulties. In this way, the child immobilizes the affected part making its muscles weak. These muscles become shorter, and due to changes in joints themselves, contractures are created and the function of muscles is gradually lost.
We apply the following in our Hospital:
- electrotherapy which relieves pain and swelling of the affected joint
- well dosed kinesitherapy (active, supported and passive exercises)
- hydrotherapy and hydrokinesitherapy for easier movements without pain
- occupational therapy
- thermo therapy – with peloid at body parts where the activity of disease allows
- laser therapy
Rehabilitation of limb injuries in children
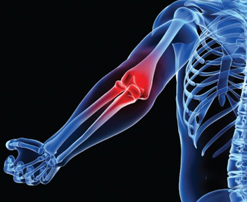
Limb injuries in children occur in all ages. Injury of arm nerves (brachial plexus lesions) may occur at birth already and this requires initiation of physical treatment in the third week of age. In older children, limb injuries may occur during falls, playing games, sports activities or in traffic. Most common injuries are in the area of elbow, hip and knee.
In addition to aforementioned causes, fractures in children also occur in various pathological conditions of bones and their locations may be in any part of bone and muscle system. These fractures are sometimes accompanied by injuries of limb blood vessels and nerves which additionally complicates and extends a treatment and rehabilitation period. Children's organism is in its growth and development stage and it has some specificities in comparison to grown ups. Some parts of children's bones are growth zones. If this zone is injured, i.e. if fracture occurs in this zone, this may result in impairment of growth, difference in length and deformities. Healing of bones is faster in children and it requires shorter immobilization period, and hence earlier initiation of rehabilitation.
Management of fractures in children is most commonly non-surgical (skin or bone traction and immobilization with plaster cast), rarely surgical (ostesynthesis with Kirschner plates, clamps).
Rehabilitation starts immediately after immobilization is removed. The aim of rehabilitation is to strengthen hypotrophic muscles which developed as a consequence of inactivity, to restore motion range in the affected joints, to restore limb function and make a child capable for normal walk without aids.

Children referred by children's surgeon and orthopedist come to Children's Department of Specialized Rehabilitation Hospital Banja Koviljaca. Upon admission, children's physician – physiatrist prepares a rehabilitation plan and program after taking history and performing examination. In order to stimulate creation of callus, healing of fracture, and strengthening of muscles, we apply certain forms of electrotherapy, laser therapy, peloid therapy, well dosed kinesitherapy and hydrokinesitherapy, and functional occupational therapy. The first steps and leaning onto the injured leg, children make in the pool, under supervision of a therapist, with gradual increase of leaning in line with healing of fracture and in line with recovery of hypotrophic muscles.
Rehabilitation takes 4 to 6 week on average.
Children come for rehabilitation with a referral of the competent physician, with the approval for rehabilitation given by the national health insurance fund, or at their parent's costs. Depending on child's age or severity of injury, usually there is a need that a child is accompanied and cared by someone. Children until 15 have right to have a carer, and if it is some severe injury, elderly children may also have a carer due to nature of disease.
Feet deformities in children

One of the most frequent congenital anomalies which develop in children are feet deformities. There are two types of feet deformities – valgus feet deformities where feet take position towards outside, and varus where feet take position towards inside. Most common valgus deformities are talus valgus, calcaneovalgus and talus verticalis, and varus deformities are metatarsus varus and equinovarus. It is important that congenital feet deformities are diagnosed in maternity hospital already, and this is done based on child's feet appearance. It is required to refer a child to children's physiatrist and orthopedist for examination as soonest.
Management of congenital feet deformities in children is non-surgical and it implies application of physical therapies which include kinesitherapies – stretching exercises, thermo therapies (paraffin), as well as introductory procedures and placing corrective plaster casts.
Physical therapies start immediately upon birth and it is considered that the first three weeks of child's life is a golden age for correction of feet deformities, because children's soft tissues are flexible under influence of mother's hormones. If physical treatment is started in the first three months, it is expected that feet deformities will be corrected in 6 to 8 weeks, and if it is started later, than the treatment takes longer. The younger is child, the better it takes physical treatment, and the structures we treat are more susceptible to the treatment and physical therapy results are better.
In few cases, if physical therapies do not yield satisfactory results, then the treatment has to be surgical. Physical treatment is applied after surgical treatment: kinesitherapy, thermo therapy (paraffin or peloid for children more than one year old), electrotherapy for scars and electrical stimulation of hypotrophic muscles.
Physical treatment of congenital feet deformities at Children’s Department of Specialized Hospital of Rehabilitation Banja Koviljaca may be done in hospital or children may come as outpatients. During rehabilitation, parents are trained to for implementation of exercises at home. There is a specially trained team for work with children, led by a children’s physiatrist, and other members are physical therapist, occupational therapist and nurses, all with higher educational level.
Pes talovalgus
It is known that normal infant’s foot appears flat because it is covered with fat tissue deposits. With foot growth and development, this fat tissue reduces, feet and underknee muscles become stronger and longitudinal arc of the foot becomes more visible. If there is heel valgus in the feet, this is a deformity that requires certain management and prevention measures.
Some children have pronounced flexibility and looseness of joints, hypotonic muscles, and in some families, more family members have different level of flat feet.
Management of congenitally impaired feet is started with exercises in a maternity hospital already, it is continued during development of a child being supervised by children’s physiatrist with occasional follow ups at children’s orthopedist. In addition to kinesitherapy which aims at strengthening of feet and underknee muscles, it is often recommended to wear shoes with the extended inner part of the heel – Thomas heel, supination wedge and reinforced medial shoe part. It is also recommended that child walks barefoot over uneven sandy or grass surface.
Hipotonio musculorum

Hypotony in newborns most frequently occurs as a consequence of baby’s suffering during passing through mother’s birth canal, but it may be seen also in children born by cesarean section. It may have a different degree, from mild to pronounced, when a child is described as being flabby as a “cloth”.
In most children being hypotonic at birth, with stabilization of the general condition, muscle tone normalizes. If hypotony remains with other pathological signs such as low spontaneous activity of a child, absence of asymmetry of normal muscle reflexes, presence or preservance of pathological primitive reflexes, positional reactions, poor weight gain, delay in motoric function development, etc, all these require diagnostics. Hypotony may be transient, but it is often a sign for some severe neuromuscular diseases. If it remains, it is necessary to have an examination by a children’s neurologist, to have some blood analyses, neurophysiological tests and only after diagnostics is done, a child with hypotony, depending on a cause, may be involved in well dosed physical treatment under supervision of children’s physiatrist.
Torticollis

Torticollis – wry neck or asymmetrical head position is often seen in children’s physiatrist’s office. Its cause in newborns is usually a forced position in the uterus during fetus development. It is usually accompanied with other position deformations and it is treated with timely kinesitherapy and positioning.
It is important to recognize and differentiate positional torticollis from torticollis within a condition with changed muscle tone (hypo or hypertony).
Recently, a benign paroxysmal torticollis has been mentioned, and this is when a child tilts its head towards one direction at some time, and during the next seizure toward the other direction. Physical treatment for such torticollis is not required, but it is important to recognize it.
The second cause, as per frequency, is injury of muscle m.SCM during childbirth. In the second-third week upon birth, on a child’s neck, or more precisely in the area of m.SCM, hard muscle swelling may be palpated (hematoma), with size from 1-3-4 cm, head inclination and limited movements, lateral flexion and turning head toward the affected side. At the end of the second and at the beginning of the third month, face and head asymmetry may be noticed. Time is very important factor here. Involvin in physical treatment in timely manner leads toward healing.
The treatment includes positioning (correction of a child’s head position with pillows or towels) which is carried out during a whole day, then application of kinesitherapy, warm paraffin overlays as an introduction to kinesitherapy and electrotherapy which is used for softening of the hematoma and tensioned and shortened muscle. The treatment may take from several weeks to a few months in three week’s series and brakes between physical therapy series. It is important to note that parents have to be familiar and involved in the positioning during sleep and corrective positions when holding a child from a very beginning.
The aim of physical therapy is to cure torticollis as soonest, latest by the first birthday. If physical therapy does not yield satisfactory results until the end of age of 1, surgical treatment is possible.
There are some other causes of torticollis, which are luckily considerably rare (neck vertebra deformations, fused neck vertebrae, tumors located in head or neck, vision and hearing problems may be torticollis causes, etc).
Physical treatment in children after birth traumas

Birth traumas in children occur during difficult and prolonged deliveries, fast deliveries, disproportion between delivery routes and fetus, hand or equipment manipulations, if fetus is too big, in case of breech birth and in deliveries when a woman gives birth for the first time.
Physical treatment of children with trauma torticollis
Trauma torticollis develops due to injuries of sternocleidomastoid muscle during difficult childbirths. Two thirds of all trauma torticollis is a consequence of the breech birth. It is characterized by hematoma appearing as a nut or plum at the joint between middle and lower third of sternocleidomastoid muscle.
It is later clinically characterized with irregular asymmetric head and neck position of a child. The head is inclined toward one side, and face toward the opposite which is a consequence of unilaterally shortening of m.SCM. In the affected side, the neck is shorter, flattened or concave.
Treatment:
1.conservative (physical therapies)
2.surgical.
Physical therapies include kinesitherapies, thermo therapies, electrotherapies. A type of therapy, duration, dose and repeating of therapy series is all defined by a physician.
Kinesitherapy is applied for preservation or increase of neck muscle length, primarily sternocleidomastoid muscle. Stretching of shortened muscles is done under control with training of parents. Child’s parents are trained to play with a child in a way to achieve symmetric behavior (sound or intensively colored toys, position of a baby in bed, carrying babe in lateral position).
Thermo therapy is in a form of paraffin therapy. It is most usually started in three weeks of age and it influences on muscle relaxation and blood circulation.
Electrotherapy is in a form of electrophoresis (potassium chloride, thyomukaze, hydrokortizon) for resorption of hematoma and prevention of muscle shortening.
Duration of the treatment for trauma torticollis is from 6 to 8 months, if the treatment is started on time (third week of age).
If physical treatment does not yield satisfactory correction (either it is started late or it is not regular), then a choice therapy is surgical (after 12 months of age).
Physical treatment of plexus brachialis injury during childbirth
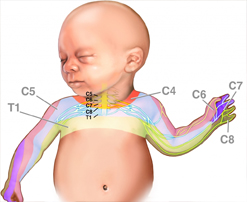
A clinical picture depends on localization of plexus brachialis injury. A child presents asymmetric posture immediately after birth. The affected arm has a specific posture characteristic for one of peripheral paralysis types: the upper paralysis, the lower paralysis or it is completely flabby in comparison to a healthy child.
The physical therapy includes kinesitherapy, thermo therapy, electrotherapy, occupational therapy and hydrokinesitherapy.
In the first three weeks upon birth, a child is left for reducing trauma consequences, swelling and bleeding. A hand is put into a position which prevents extension of injured plexus brachialis roots and accelerates healing of trauma consequences (positioning). Parents are trained to position a hand and to change its position every 2-3 hours.
Kinesitherapy is started after 3 weeks upon birth. The aim is to strengthen muscles of shoulder and blades, as well as of the affected arm and preservation or improvement of motion range in joints (passive and active exercises).
Thermo therapy (paraffin therapy, peloid therapy for children older than 1 year).
Electrotherapy implies electrical stimulation of the affected muscle which may be preceded with longitudinal galvanization. Electrical stimulation is done until the second year of age.
Occupational therapy: a therapist uses various methods and means to activate the affected arm. Occupational therapy may be through a game (selected toys – rattles, balls, cubes, phone, clock, moving toys, scissors, pens, typewriters).
Hydrokinesi therapy in the pool or bath – making movements within water. Movements are facilitated in water and these are made in order to strengthen paretic muscles and for overcoming joint contractures.
Physical treatment in a specialized rehabilitation institution such as Specialized Rehabilitation Hospital Banja Koviljaca contributes to better and faster recovery of children with birth trauma of plexus brachialis and torticollis. If physical treatment is initiated on time and if it is done long enough, physical treatment results are good in children.
